INTRODUCTION
Osteoporosis is a medical disorder characterized by a generalized low bone mass and fragility with a consequent increase in fracture risk, particularly of vertebrae, hip and wrist.[1] It is a physiological gender and age-related condition resulting from bone mineral content loss and structural changes in bones.[2,3] Charles Dent said that “senile osteoporosis is a pediatric disease,” meaning that failure to achieve adequate peak bone mass during adolescence increase the risk of osteoporosis in later life.[2]
There are two types of osteoporosis: (1) Postmenopausal osteoporosis caused by cessation of estrogen production and characterized by spinal fracture and (2) Osteoporosis that affect the older population and results in proximal femur fracture.[4]
Nutrition is a modifiable factor that plays an important role in determining peak bone mass. Appropriate and adequate nutrition of elderly people is a great importance for their general and oral health. Diet plays an important role in preventing disease in elderly.[5,6] Diet and dentition are of great importance, due to a significant role of diet in etiology of common systemic diseases such as bowel cancer and coronary heart disease, especially in elderly.[7] It is very much alarming for a geriatric population especially in developing countries such as Bangladesh, India, Nepal and almost south Asian territory.
Osteoporosis is asymptomatic until the clinical sequels (fracture) occur. These fractures and their consequences cause pain, disability, deformity and sometimes premature death. Currently, osteoporosis diagnosis and staging are based on the identification of different risk factors, the most important being low bone mineral density (BMD) of the femoral neck or lumbar spine. World Health Organization has been an established the diagnostic level of BMD <−2.5 for defined as osteoporosis.[8] Bisphosphonates are approved to treat osteoporosis and are frequently used to treat osteopenia as well.[9,10] Zoledronic acid at a dose of 5 mg yearly for 3 years is most potent, safe and effective in osteoporotic patient.[11-15] They are also used for a variety of less common conditions such as Paget’s disease of bone and osteogenesis imperfecta of childhood.[9,16] By far the most prevalent and common indication, however is osteoporosis.[17,18] Osteoporosis may arise in the context of other diseases such as inflammatory bowel disease or primary biliary cirrhosis, as a result of medication, most commonly steroids or as a consequence of postmenopausal aging.[19-21]
Alveolar bone is a unique tissue representing the mast viable part of the tooth-supporting apparatus.[5,22] The consequences of aging often involve the risk of osteoporosis, leading to an impaired quality-of-life of the elderly patient.[23] Morphology and functional oral sequel of aging be well-documented in the dental literature, but not those resulting from osteoporosis. Many of the studies have cited the possible correlation between age, systemic osteoporosis, periodontal disease, tooth loss and changes in quantity and quality of bone of the maxillae and mandible.[24,25]
Digital radiographs are an increasingly popular option in the clinic. Such images are composed of pixel with a specific numerical value for each one. Two important methods of evaluating the pixel in these images are fractal dimension and pixel intensity (PI).[7,10] PI is a gray scale measure, ranging from zero (black) to 256 (white) in a digital image. Areas of bone lose represented as darker areas while areas of bone gain represented as a lighter area.[10,25] The mandibular bone mass (MABM) by the mean gray level values of the alveolar bone on digital radiograph. The restoration of occlusion for partially and totally edentulous patient often requires adequate bone therapy. Consequently, the frequent use of an implant supported prosthesis for the elderly patient who is routinely or potentially osteoporotic demand a better understanding of the relationship between osteoporosis and the stomatognatic system. The aim of this study was to see the improvement of MABM in postmenopausal osteoporotic patient treated with zoledronic acid.
MATERIALS AND METHODS
Totally 150 postmenopausal osteoporotic patients were selected for study. 100 patients were freshly diagnosed as osteoporotic condition named Group A. Rest 50 patients were treated osteoporotic condition named Group B. All treated osteoporosis patient had been taken aclasta (zoledronic acid) in intravenous route (5 mg once a year) for treatment before 1 year. Primary postmenopausal women more than 50 years of age with BMD −2.5 or less who given consent, none other secondary factors related to osteoporosis and postmenopausal osteoporotic patients those treated by zoledronic acid were included in this study. Patients with suspected condition affected bone mineralization were excluded from this study. All procedure was followed for both groups.
Osteoporosis diagnosis by dual-energy X-ray absorptiometry (DEXA) scans from Comilla Medical College, Comilla. BMD at the lumbar spine and femoral neck were measured by DEXA scanner.
Digital radiograph-after the clinical examination, periapical radiographs were taken using radiovisiography (RVG). RVG are manufactured by Gendex, USA. Vixwin platinum image processing software is used for the measurement of gray level of bone. The MABM were measured from gray value. The site between the premolars was used as “standard site” for the region of interest (ROI). The ROI was set on the apical radiograph with “rectangular tool” avoiding the lamina dura and the most crestal locations. No apical bone was included.[25] Then the gray value were measured from low level to high level (by assigning the value zero to black 256 to white). Areas of bone loss represent as darker whereas areas of bone gain represented as lighter areas.[25] This obtained data are presented as mean ± standard deviation, and it was posted to data sheet for statistical analysis.
Calculation of mean and standard deviation, as well as correlation and difference, were performed using SPSS 11.5 for windows (Windows XP). A P < 0.05 were considered to be statistically significant.
RESULTS
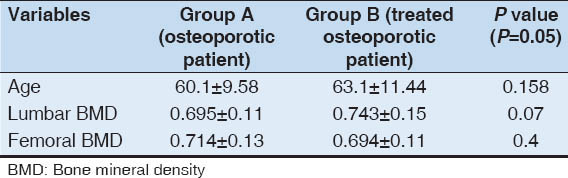
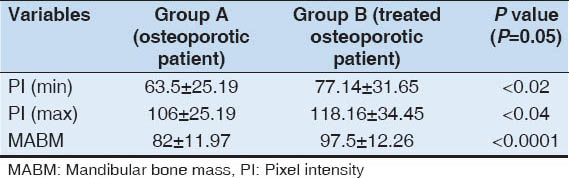
The mean age of an osteoporotic patient and treated osteoporotic patient are statistically non-significant [Table 1]. The lumbar spine and femoral neck BMD were 0.706 ± 0.11 and 0.723 ± 0.12, 0.743 ± 0.15 and 0.694 ± 0.11 respectively in osteoporotic patient (Group A), treated osteoporotic patient (Group B). Those were statistically non-significant. Minimum level of PI in Group A and Group B was statistically significant [Table 2]. The mean PI (min) were 62.28 ± 26.37 and 77.14 ± 31.65 in Group A and Group B. Maximum level of PI in both groups was also statistically significant [Table 2]. The mean PI (max) was 102.82 ± 30.03 and 118.6 ± 34.44 in Group A and Group B. The MABM in treated group was 97.5 ± 12.26 and non-treated group was 82 ± 11.97. Those were statistically strongly significant different (P < 0.0001) between two groups [Table 2].
Table 1
Age, lumbar spine and femoral neck BMD
Table 2
PI of mandibular bone and presenting teeth
DISCUSSION
In this study, we found that the mean lumbar and femoral BMD of an osteoporotic patient and treated osteoporotic patient was non-significantly different. Although pixel value of both groups was significantly different. Minimum and maximum level of pixel level was more in treated group rather than non-treated group. As no other study has found the pixel value of an osteoporotic patient and treated osteoporotic patient. It is difficult to compare our results with those from other studies. However, there were some other studies found a strong correlation between BMD and pixel value.[26,27] In clinical trials, bisphosphonate like alendronate has been found to reduce the risk of progressive loss of alveolar bone.[28]
In this study, we also found the MABM in treated group was higher than non-treated group. This difference was statistically strongly significant. Zoledronate like bisphosphonate was used for treatment of osteoporosis in this studied patient. Bisphosphonate maintain trabecular micro-architecture of bone in post-menopausal women. The degree of mineralization of bone matrix is a determinant of bone strength.[29] In other study found that bone mineral content were significantly increased in therapeutic treatment by etidronate.[3] Zoledronate, i.e., an annual intravenously administrated bisphosphonate showing an increase in activity of osteoblast rather than the mean degree of mineralization.[11] Alveolar bone develops as a membrane bone.[30] There are minor phenotypic difference between osteoblasts depending on their site of origin and anatomical location, which can be demonstrated biochemically.[31] Membrane bone osteoblasts also have an increased rate of cell division as compared to iliac crest osteoblast.[32] For this reason femoral and lumbar BMD of both groups were non significantly different but pixel value and MABM were significantly different.
The rectangular tool, used when the pixel value was assessed, included a larger area than the circle. It was placed halfway between the crest and the apical area, which is the area shifting from a denser cervical trabeculation to a sparse trabeculation.[25] Whereas in osteoporosis in cortical bone result in an increased number of lacunae and porosity and later on thinner cortical plates[6,33] it leads to larger intertrabecular spaces and thinning of the trabeculae in the cancellous bone.[34] The mineral content is also decreased in a certain area ROI and therefore also the pixel value of radiographed area is decrease. MABM was improved in zoledronic acid treated group that was measured from significantly increased PI.
Digital periapical radiograph by RVG was used due to their minimal radioactive emission and high image quality that are not lost upon digitalization. The rectangular tool, used when the pixel value was assessed, included a larger area than the circle. It was placed halfway between the crest and the apical area, which is the area shifting from a denser cervical trabeculation to a sparse trabeculation.[25] The ROIs were set on the apical radiograph of the individual on the 6 mm step of the reference radiograph with “rectangular tool” avoiding the lamina dura and the most crestal locations. No apical bone was included. Whereas in osteoporosis in cortical bone result in an increased number of lacunae and porosity and later on thinner cortical plates[6,24] it leads to larger intertracular spaces and thinning of the trabeculae in the cancellous bone.[25] The mineral content is also decrease in a certain area ROI and therefore also the pixel value of radiographed area is decrease. On the other hand treated osteoporosis had been shown to increase the pixel value in a certain area ROI.
CONCLUSION
This study showed significant improvement of MABM and also improvement of lumbar BMD in postmenopausal osteoporotic patient treated with zoledronic acid. Large scale prospective studies are necessary to make an effective conclusion.